Partnerships a COVID silver lining
Thinking about the unprecedented global health crisis of this pandemic, the words of poet John Donne come to mind, and are as compelling today as when he wrote them 400 years ago. To paraphrase: no one is an island, we all need to be part of a community to thrive.
That has certainly been the case for peopleCare Communities. Our goal was to save lives and support our compassionate, caring frontline care teams to balance resident safety and quality of life. Our partnerships – longstanding and new – made this possible.
Megan Allen-Lamb is President of peopleCare. She says one silver lining of the COVID-19 pandemic is how it accelerated change and created an openness to collaborate for the greater good.
“While partnerships have always been a peopleCare strength, our journey to support our residents, staff, families and partners during this pandemic took us down some amazing paths,” says Allen-Lamb. “How people and organizations came together to help and inspire one another is the story, the legacy and the opportunity of this past year. We’ve truly been stronger, together.”
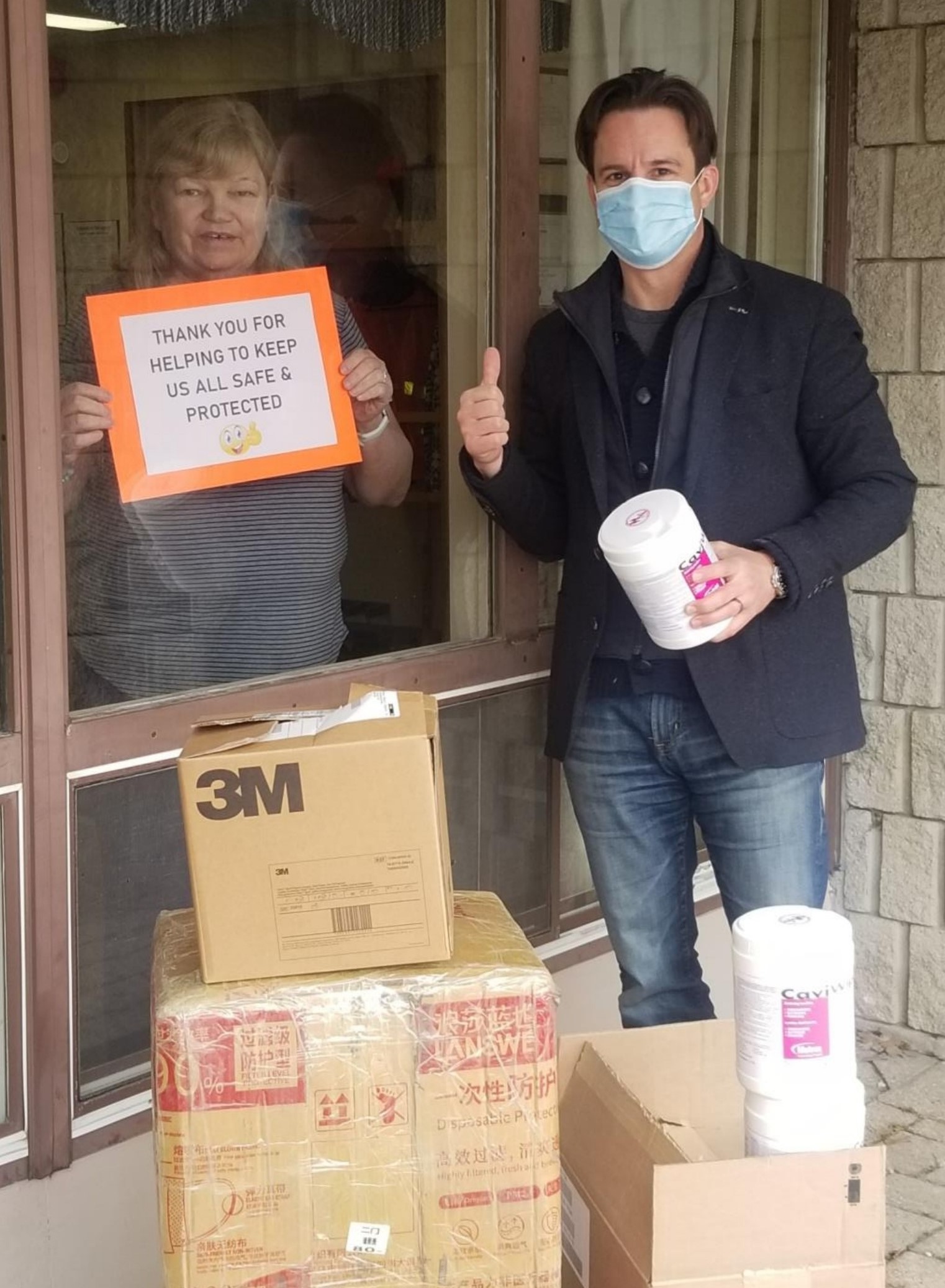
With the motto “No One Left Behind,” peopleCare Chairman and CEO Brent Gingerich sourced and delivered PPE to peopleCare homes and others in Ontario
Our shared goal
As our long-term care teams led with heart through these uncharted COVID times, our hospital partners were beside us every step of the way: connecting on our outbreak contingency planning, checking in on shared concerns like staffing and personal protective equipment (PPE), and working with our skilled infection control leads to ensure practices were evidence-based and top notch.
The learnings went both ways. Perry Lang is CEO of Woodstock General Hospital, where he has worked for over 20 years. He recalls his staff coming back from one long-term care home with a better understanding of the challenges of care and infection control in long-term care homes.
“Both long-term care and hospital staff have a high degree of expertise relating to the patients they serve,” says Lang. “Our staff learned valuable lessons working at long-term care homes during this pandemic, including developing a deeper appreciation for the different needs of long-term care residents.”
The hospital compiled a list of staff willing to work in long-term care homes in an outbreak if needed. This foresight and commitment to supporting the community meant peopleCare was able to find a registered nurse to work alongside our team during a tough outbreak.
“This one clinical resource allowed us to honour our ill residents’ wishes and continue to meet their increased care needs in the comfort of their own home,” says Jenn Killing, Vice President Quality, Research and Strategic Partnerships at peopleCare. “It was exactly what we needed, at exactly the right time.”
With the focus on creating new models of interconnected care, such as Ontario Health Teams, in the past decade, healthcare organizations of all types are gaining a better understanding of one another’s role as system partners. There is also more appreciation of how working as a system benefits everyone in the community by providing the right care at the right time by the right provider.
The bottom line: every long-term care home should consider making the first move to connect with all of their local health system partners before a crisis makes it necessary. “At the end of the day, we’re all working hard to meet the needs of aging seniors in our community; that’s our shared goal,” says Killing.

peopleCare partnered with local business to thank staff during Caregiver Week
Friend-raising
Establishing meaningful relationships with organizations like Family Councils Ontario (FCO), the Ontario Association of Residents’ Councils and the Ontario Caregiver Organization (OCO) has been essential in peopleCare’s ability to quickly bring new resources into our homes this past year.
For peopleCare, the value of partnering with families is the mutual trust and dedication it develops toward keeping the well-being of residents at the heart of all we do and the decisions we make together. We talked with FCO early on about safely bringing families back into long-term care homes. They also provided feedback on our Family Survey, which informed our plans for safe, socially distanced visits and improved communication and gave us an opportunity to connect with any family wanting more engagement and support.

Balancing safety with quality of life is a continued focus throughout this pandemic at all peopleCare homes
A flourishing partnership enabled peopleCare’s work as an early adopter of OCO’s Partners in Care toolkit (see more at ontariocaregiver.ca/partnersincare and peoplecare.ca). We have been pleased to be part of the learning collaborative established by OCO that includes members from long-term care, hospitals, Ontario Health Teams and provincial partners.
Amy Coupal is CEO of the OCO. She says the collaborative has emerged as a hub of cross-sector learning for family caregiver engagement – both during COVID and for the long term – which speaks to the value participants find in sharing barriers and lessons learned. “There’s magic in peer-to-peer learning,” Coupal says. “It’s reassuring to see it is possible to meaningfully and safely engage caregivers during a pandemic.”
No wrong turns
It has been said that creativity is the antidote to an unhealthy response to a crisis. As peopleCare’s frontline teams were going all out to care for residents, with an outpouring of support from families and community (including donating essential PPE and supplies), our leaders were reaching to the four winds looking to be inspired by new opportunities and team-ups.
Leading alongside other innovators and government is always a priority for peopleCare, and never more so than during a pandemic. We were pleased to pilot rapid tests and help shape future testing solutions. We connected with universities trialling early COVID interventions. We even partnered with Canada’s National Ballet School to pilot and evaluate virtual creative movement classes, codesigned with Baycrest, for residents to enjoy while socially distanced.
With so much confusion and anxiety in the early days of COVID, peopleCare reached out to Doctors Without Borders (DWB), to leverage their expertise as international leaders in infection control, to protect our staff and residents.
Enter Jaime Wah, Medical Lead for DWB’s Canadian COVID-19 Response Team, and a Registered Nurse who knows a thing or two about fighting infectious illnesses. After giving our infection prevention practices a big thumbs-up, Wah reassured our staff, through a live webinar during National Nursing Week, “You have the tools to save lives: trust in your training, trust in your PPE.”
We also sought DWB’s input into our family visiting protocols. After all, we thought, if you can visit in Ebola, you can visit in COVID.
The path forward
Heard about the “great snap-back” yet? It is what some psychologists predict will happen when enough people are COVID-immune that society feels safe in rushing back into old social norms and behaviours.
Speaking strictly from a partnership perspective, if we want to keep momentum building and maximize the acceleration of strategic collaboration that happened during COVID, health organizations cannot simply go back to doing exactly what we were doing before once the pandemic is behind us.
The long-term care sector is primed to continue leading as a partner for government and positively shaping the future of the health system. Transformation will also take sustained, imaginative and solution focused cooperation with a diversity of contributors who share a vision to improve resident care and quality of life, support our staff and build even better relationships with our families.
That our greatest successes happen when we face and resolve our shared challenges together is something Allen-Lamb cannot stress enough. “The past year has been a masterclass in the value of building relationships and partnering within and outside our sector,” she says.
“The path forward that most benefits our residents, staff, families and communities is undeniably the one we take together.”
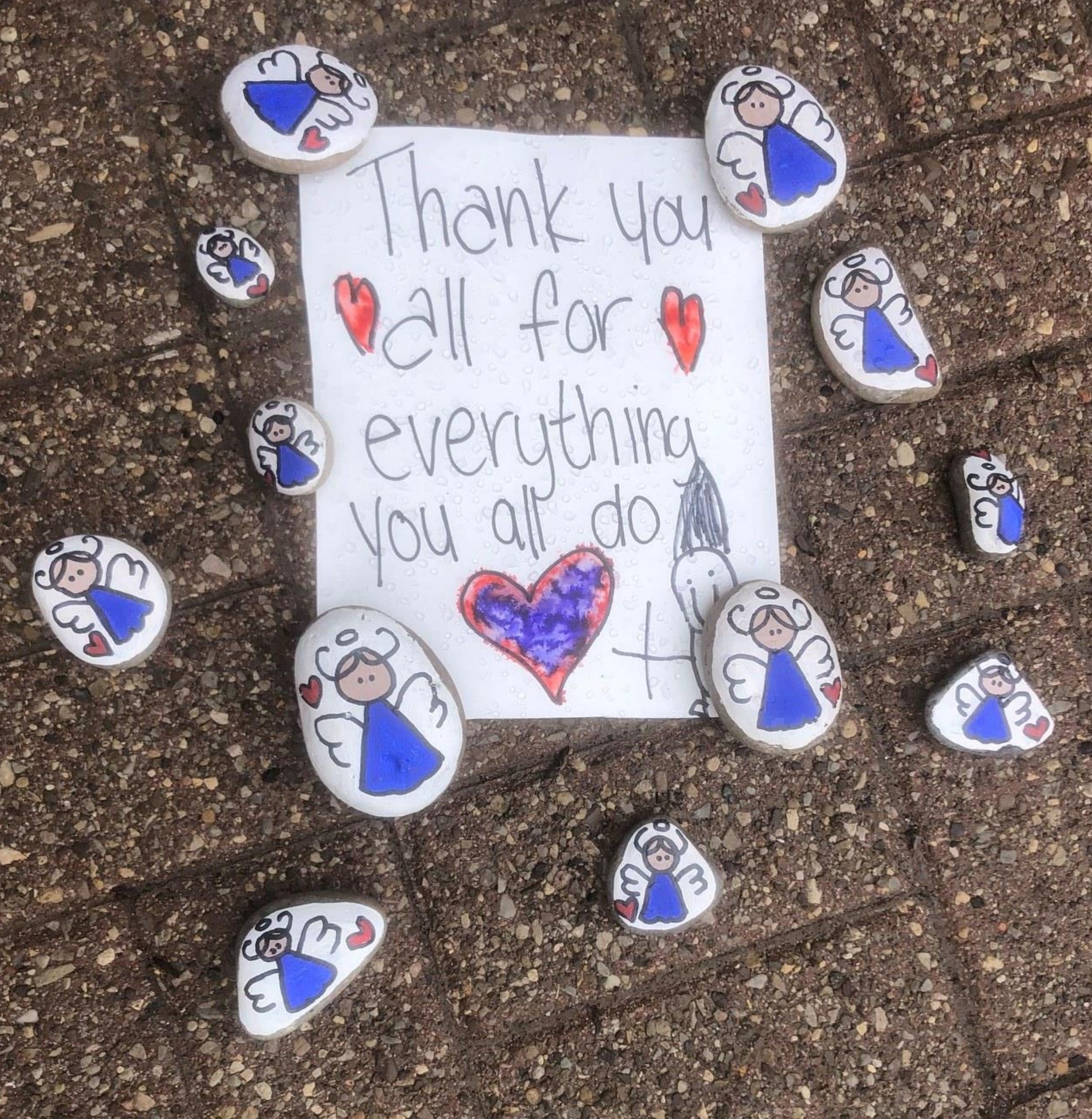
Our communities supported our Homes with encouragement and kindness, like these touching rocks and note from a local 8-year old boy, left outside a peopleCare home
—
Article written by Sheena Campbell, Vice President of Communications and Engagement at peopleCare Communities. First published in the Spring-Summer 2021 issue of OLTCA’s magazine, Long Term Care Today, available here.
Printable version of article available here.